How effective are non-medical masks? A scientific view of a much-discussed question


Your consent to the storage of data ('cookies') is required for the playback of this video on Quickchannel.com. You can view and change your current data storage settings at any time under privacy.
- Several DLR institutes launched a collaborative project to investigate the effectiveness of fabric masks.
- The findings clearly show their positive contribution, although smaller aerosols can still penetrate the fabric.
- This project was based on technology that is normally used to examine airflows in the aerospace industry.
- Focus: Medicine
Non-medical masks are an important part of the fight against the Coronavirus pandemic. The latest research shows how human breath is deflected when wearing a mask and how this distributes the aerosols contained in the exhaled air.
Several institutes within the German Aerospace Center (Deutsches Zentrum für Luft- und Raumfahrt; DLR) came together in an interdisciplinary, collaborative project to investigate the functioning and effectiveness of non-medical fabric masks. The experiments clearly show how wearing a non-medical mask influences the distribution of exhaled aerosols and how this contributes to preventing the spread of infection.
Filtering and aerodynamic effects
The first evaluation of experimental data provides a clear impression of how the masks work.
"The tests plainly demonstrate the positive effect of non-medical masks, although smaller aerosols can still penetrate the fabric," says Andreas Schröder from the DLR Institute of Aerodynamics and Flow Technology and the Principal Investigator of the research. A significant proportion of exhaled bioaerosols measure less than five micrometres across, but the mesh size in fabric masks is considerably larger. The aerosols pass almost unobstructed through the mesh in the investigated masks and are then carried via air currents. However, fabric masks are still effective, as they slow down and deflect the exhaled breath. Laboratory tests show that mouth and nose masks effectively decelerate the exhaled flow of air containing the aerosols.
The thermal effect of body heat makes potentially infectious particles – which remain close to the body due to the mask in calm indoor air – float towards the ceiling, where they follow the air flow and spread slowly through a room. This means that the aerosols travel further through space and are affected by turbulence in the air, which lowers their potency even more. The masks lead to a drop in concentration of any infectious aerosols, which particularly protects those in close proximity. It is nevertheless important to ventilate rooms on a regular basis to prevent any accumulation of possible bioaerosols. From a physical perspective, the volume increases with the third power of the distance (that is, the number of cubic metres), which reduces the concentration of bioaerosols. This is why it is still advisable to adhere to social distancing when wearing a mask.
Methodology
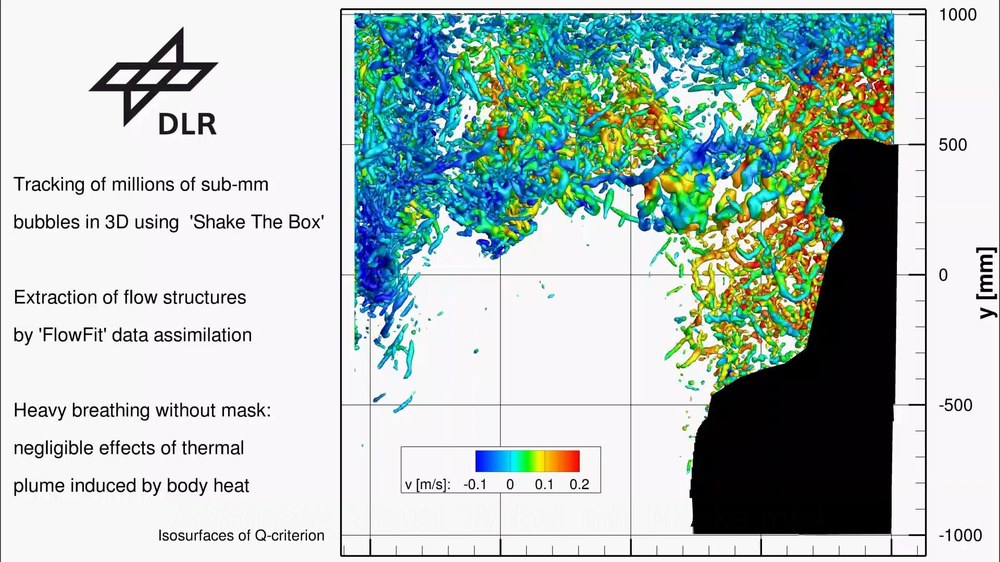
The imaging methods developed at the DLR Institute of Aerodynamics and Flow Technology are usually used for flow investigations in aerospace applications. DLR’s proprietary '3D Particle Tracking' technology has been applied in the Aeromask project to research the spread of the infectious SARS-CoV-2 virus. This technology enables precise tracking – at a scale of just a few millimetres – of exhaled airflows, their deflection by masks and the consequent transport of aerosols through closed indoor environments measuring several cubic metres. The pathways are visualised to illustrate the dynamic distribution of potentially infectious aerosols and particles in the room.
In the first phase of the project, the flow of exhaled breath and ambient air and the influence of different masks was investigated. For this purpose, an experimental space measuring 12 cubic metres was flooded with very small soap bubbles the size of sugar grains (diameter approximately 350 micrometres). Filled with a mix of helium and air, the bubbles remained suspended for long periods and followed the complex flow field in the test room.
A seated test dummy breathed in the test room. Its artificial lung created a cyclic air flow that replicated that of a human being. A built-in heater simulated body warmth and induced the associated thermal currents in the surrounding air.
High-resolution camera technology
Several high-resolution streaming cameras – each with an image size of 50 megapixels – captured the movement of the soap bubbles, which were illuminated with pulsed light from a large array of LEDs.
To conduct the analyses, the researchers developed sophisticated volumetric evaluation and data assimilation methods that tracked the trajectories of the millions of individual bubbles over time as they travelled through the test room. DLR's proprietary 'Shake-The-Box' (STB) particle tracking technique used a small number of cameras to reconstruct a very large number of their 3D trajectories in the flow, based on time-resolved images of these small bubbles. STB technology makes optimum use of the time information contained in the particle images for 3D reconstruction, whereby approximately ten times more particle trajectories can be followed in the measurement volume, compared with previous particle tracking methods.
Further project phases
Following completion of the laboratory phase, the project will move on to two more stages to acquire greater understanding of the infectiousness and movement of the aerosols as they spread through the room. In a next step, the DLR Institute for Software Technology will use the measurement data to prepare a simulation and visualisation of how the aerosols and particles move through the air. The properties of simulated bioaerosols (defined mixtures of various micro-organisms) and their interaction with masks will be investigated by the Space Microbiology Research Group at the DLR Institute of Aerospace Medicine.
The findings of the next research phases in the Aeromask project will be released in spring 2021.
